COVID-19’s repercussions on the brain are causing concern over potential long-term consequences, including an increased susceptibility to Alzheimer’s disease. Moreover, there’s an indication that the interplay of brain inflammation and Alzheimer ‘s-related conditions might heighten the risk of severe COVID-19 infection.
A recent study unearthed alterations in the transcriptomic patterns within human olfactory mucosal cells among individuals with Alzheimer’s who contracted COVID-19.
This discovery suggests a potential link that could exacerbate the impact of COVID-19 in those already grappling with Alzheimer’s. The study, a collaborative effort between the University of Eastern Finland and the University of Helsinki, sheds light on these intricate connections.
What is Alzheimer’s Disease?
Alzheimer’s disease is a brain disorder that slowly erodes memory and cognitive abilities, eventually harming the capacity to perform even basic tasks.
Over time, the condition worsens, denoted by alterations in the brain resulting in the assemblage of specific proteins. This process leads to the shrinking of the brain and the eventual demise of brain cells.
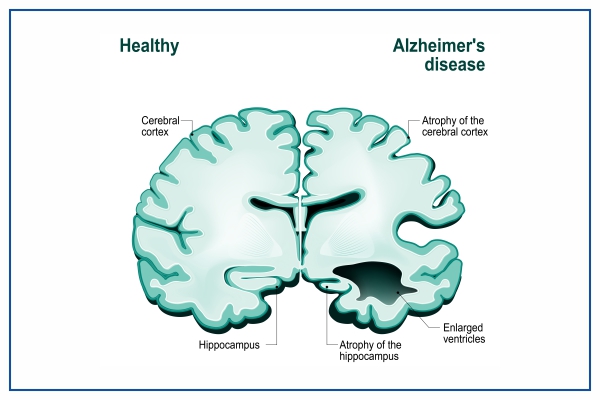
Alzheimer’s is the predominant cause of dementia, a condition characterised by a gradual decline in memory, cognitive function, behaviour, and social skills. These changes significantly impact an individual’s ability to carry out daily functions.
What is the Study about?
The impetus behind the study stemmed from apprehensions about how COVID-19 impacts individuals with pre-existing conditions like Alzheimer’s disease (AD).
Olfactory dysfunction, marked by a diminished sense of smell, is a frequent occurrence in COVID-19 cases and is also prevalent in individuals with AD. Delving into the olfactory mucosa as a direct conduit linking the external environment to the brain, the research sought to scrutinise the interplay between SARS-CoV-2 infection and AD within the olfactory mucosa.

The goal was to assess the olfactory mucosa’s potential as a conceivable entry point for the virus into the brain.
How was the study conducted?
The study harnessed a 3D in vitro model of the olfactory mucosa, employing primary cells sourced from willing participants, encompassing both cognitively sound individuals and those diagnosed with AD.
These cells underwent cultivation at the air-liquid interface (ALI), a technique offering a controlled setting mirroring physiological conditions closely.
The collaboration with Kuopio University Hospital facilitated the gathering of olfactory mucosal biopsies.
This interdisciplinary investigation seamlessly integrated insights from molecular and cellular biology, neurology, and virology, aiming to decipher the repercussions of various SARS-CoV-2 variants on the olfactory mucosa.
Results of the Study
Contrary to predictions, cells derived from healthy individuals and those with AD displayed akin susceptibility to SARS-CoV-2 infection, indicating no discernible contrast in initial infection rates between the two groups.
However, a notable disparity surfaced in the gene activity of infected cells from individuals with AD. Their cells exhibited heightened oxidative stress, altered immune responses, and substantial changes in genes associated with olfaction compared to olfactory mucosal cells from cognitively healthy counterparts.
According to Ali Shahbaz, a doctoral researcher in Professor Katja Kanninen’s research group at the University of Eastern Finland and the study’s first author, “The results imply a conceivable scenario where individuals grappling with AD could encounter more severe COVID-19 outcomes, possibly due to pre-existing inflammation in the olfactory mucosa.”
Also Read : Lipids and Type 2 Diabetes: New Research Reveals Close Connection Between Them












Comments 2