Cervical cancer, originating from the cervix (the lower part of the uterus that connects to the vagina), is a global health concern, particularly in low- and middle-income countries. It ranks as the fourth most prevalent cancer among women worldwide. Alarmingly, India contributes to a significant portion of this, accounting for a quarter of all cases. Each year, India records about 1,22,844 new cases, making a substantial contribution to global cancer deaths. In 2020 alone, there were approximately 604,000 new cases and 342,000 deaths worldwide from this disease. The impact of the cancer is indeed profound and calls for urgent attention and action.

Women need to know
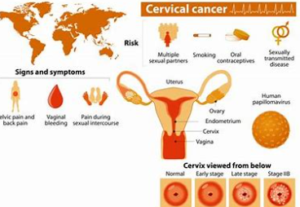
The Human Papilloma Virus (HPV) is a key player in the onset of this cancer. It’s the most common viral infection of the reproductive tract, and most women who are sexually active will contract it at some point. There are over 100 types of HPV, but about 14 strains are high-risk and can lead to cancer. The cancer is categorized based on the type of cell in which the cancer begins. The main type of cervical cancer is Squamous cell carcinoma, which begins in thin, flat cells (squamous cells) that line the outer part of the cervix. While most infections clear up within two years without intervention, some high-risk strains can persist and progress to cervical cancer.
If an HPV infection in the cervix isn’t treated, it can cause 95% of cervical cancers. It usually takes 15–20 years for abnormal cells to become cancerous, but this process can be faster (5–10 years) in women with weakened immune systems, such as those with untreated HIV.
Women living with HIV are six times more likely to develop this cancer than the general population. Other risk factors include the oncogenicity grade of the HPV type, immune status, the presence of other sexually transmitted infections, number of births, young age at first pregnancy, hormonal contraceptive use, and smoking.
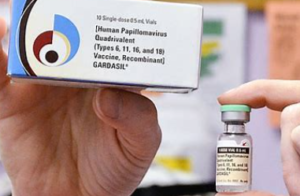
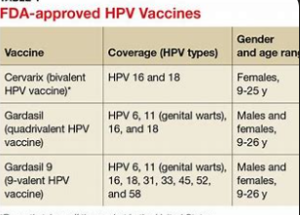
Prevention and Vaccination: Prevention is better than cure, and this is particularly true for cancer. HPV vaccines, such as Gardasil 9, are now available in India and offer protection against seven high-risk strains that cause cancer and two strains that cause genital warts. If all girls receive the vaccine before they become sexually active, we could see a significant reduction in cervical cancer cases.
After Cervical Cancer
Surviving the cancer doesn’t mean the end of a normal life. Women who become pregnant after treatment are closely monitored throughout their pregnancy. A renowned doctor has shared insights on the potential risks, preventive measures, and treatment procedures for pregnancy post-recovery.
And remember, early detection is key. All women between the ages of 21 and 65 should have regular pap smears every three years.
Prioritizing Cervical Health in 2024
The Cervical Cancer Awareness Month in 2024, marked in January, holds a multi-dimensional significance. The theme “Learn, Prevent, Screen” underscores the importance of education about cervical cancer risks and the life-saving role of regular screenings. It also highlights the critical preventive measure of HPV vaccination. This month is dedicated to raising awareness about cervical health, emphasizing prevention, early detection, and the importance of regular screenings.
The National Cervical Cancer Coalition (NCCC) initiated this awareness month over a decade ago to combat the cancer prevalence and emphasize preventive measures. The World Health Organization (WHO) Global Cervical Cancer Elimination Initiative is also highlighted during this month. These collective efforts aim to empower individuals to prioritize their well-being and cervical health.
Empowering Cervical Cancer Prevention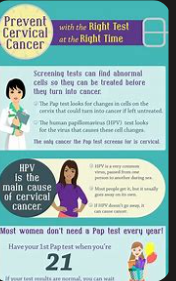
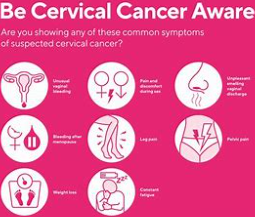
Empowerment is a key element in the prevention of cervical cancer. By equipping women with precise information about the risk factors, symptoms, and screening options, we can facilitate them to make knowledgeable decisions about their health. The availability of healthcare services, education, and support networks are essential parts of this empowerment.
Despite the progress in increasing awareness and broadening access to preventive measures, substantial challenges remain. Obstacles such as stigma, misinformation, and limited resources continue to impede the fight against this cancer. Nevertheless, the progress in medical technology, heightened advocacy, and collaborative partnerships provide optimism for surmounting these hurdles.
Healthcare providers have a significant role in advancing cancer awareness and prevention. They can empower women to prioritize their health by providing all-encompassing information, promoting regular screenings, and addressing concerns with understanding and empathy.

Cervical Cancer Awareness Month serves as a poignant reminder of the impact of this disease and the importance of proactive measures. Let us join together in raising awareness, promoting preventive care, and supporting those affected by this disease. Together, we can make strides towards a future free from the threat of this cancer.











